Search
- Page Path
- HOME > Search
- Calcium & bone metabolism
- Familial Correlation and Heritability of Hand Grip Strength in Korean Adults (Korea National Health and Nutrition Examination Survey 2014 to 2019)
- Seong Hee Ahn, Eun Byeol Park, Seongha Seo, Yongin Cho, Da Hea Seo, So Hun Kim, Young Ju Suh, Seongbin Hong
- Endocrinol Metab. 2023;38(6):709-719. Published online November 7, 2023
- DOI: https://doi.org/10.3803/EnM.2023.1740
- 1,201 View
- 48 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
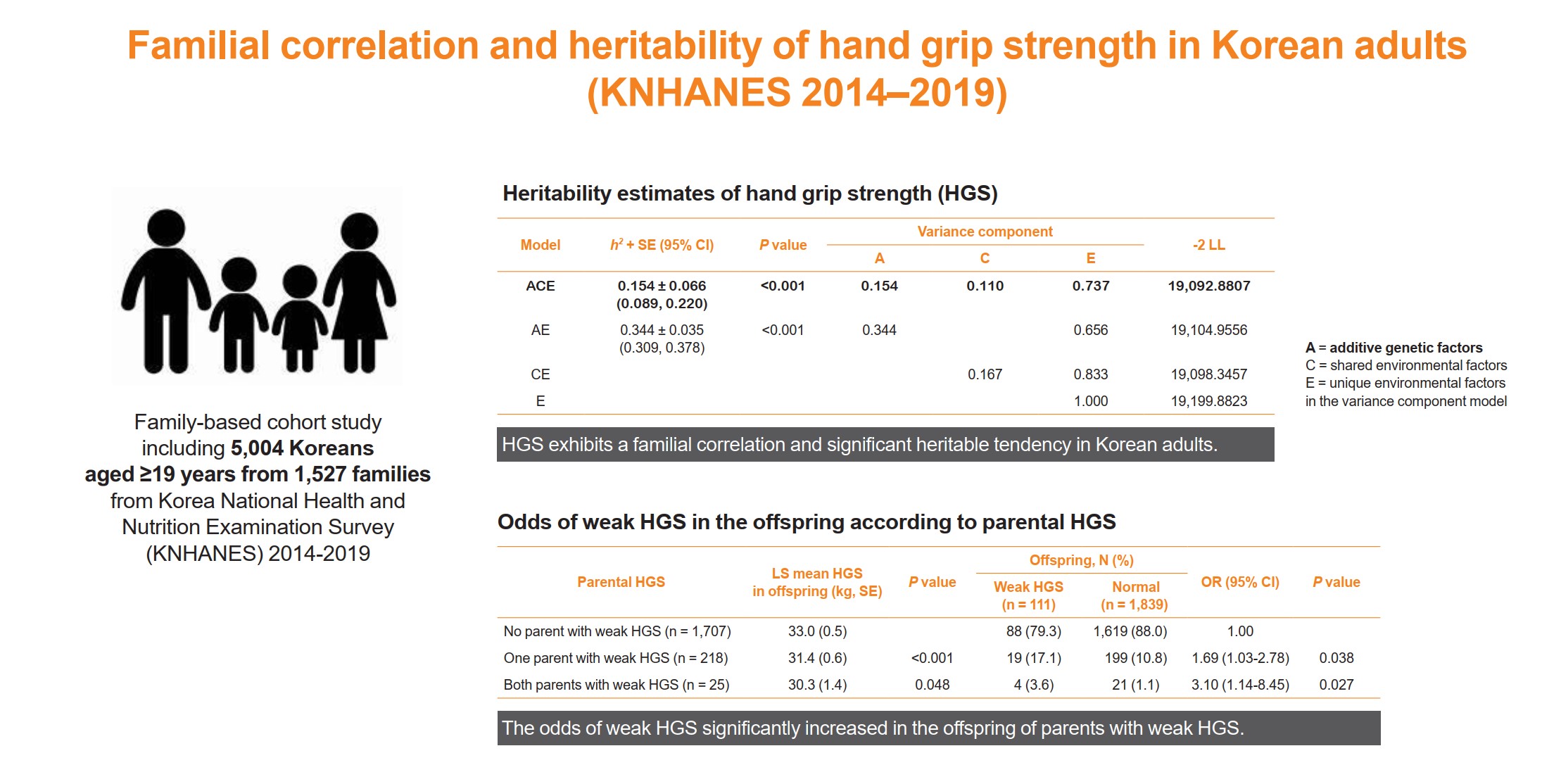
The onset and progression of sarcopenia are highly variable among individuals owing to genetic and environmental factors. However, there are a limited number of studies measuring the heritability of muscle strength in large numbers of parent-adult offspring pairs. We aimed to investigate the familial correlation and heritability of hand grip strength (HGS) among Korean adults.
Methods
This family-based cohort study on data from the Korea National Health and Nutrition Examination Survey (2014 to 2019) included 5,004 Koreans aged ≥19 years from 1,527 families. HGS was measured using a digital grip strength dynamometer. Familial correlations of HGS were calculated in different pairs of relatives. Variance component methods were used to estimate heritability.
Results
The heritability estimate of HGS among Korean adults was 0.154 (standard error, 0.066). Correlation coefficient estimates for HGS between parent-offspring, sibling, and spouse pairs were significant at 0.07, 0.10, and 0.23 (P<0.001, P=0.041, and P<0.001, respectively). The total variance in the HGS phenotype was explained by additive genetic (15.4%), shared environmental (11.0%), and unique environmental (73.6%) influences. The odds of weak HGS significantly increased in the offspring of parents with weak HGS (odds ratio [OR], 1.69–3.10; P=0.027–0.038), especially in daughters (OR, 2.04–4.64; P=0.029–0.034).
Conclusion
HGS exhibits a familial correlation and significant heritable tendency in Korean adults. Therefore, Asian adults, especially women, who have parents with weak HGS, need to pay special attention to their muscle health with the help of healthy environmental stimuli.

- Clinical Study
Big Data Articles (National Health Insurance Service Database) - Effect of Teneligliptin versus Sulfonylurea on Major Adverse Cardiovascular Outcomes in People with Type 2 Diabetes Mellitus: A Real-World Study in Korea
- Da Hea Seo, Kyoung Hwa Ha, So Hun Kim, Dae Jung Kim
- Endocrinol Metab. 2021;36(1):70-80. Published online February 24, 2021
- DOI: https://doi.org/10.3803/EnM.2020.777
- 4,976 View
- 192 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
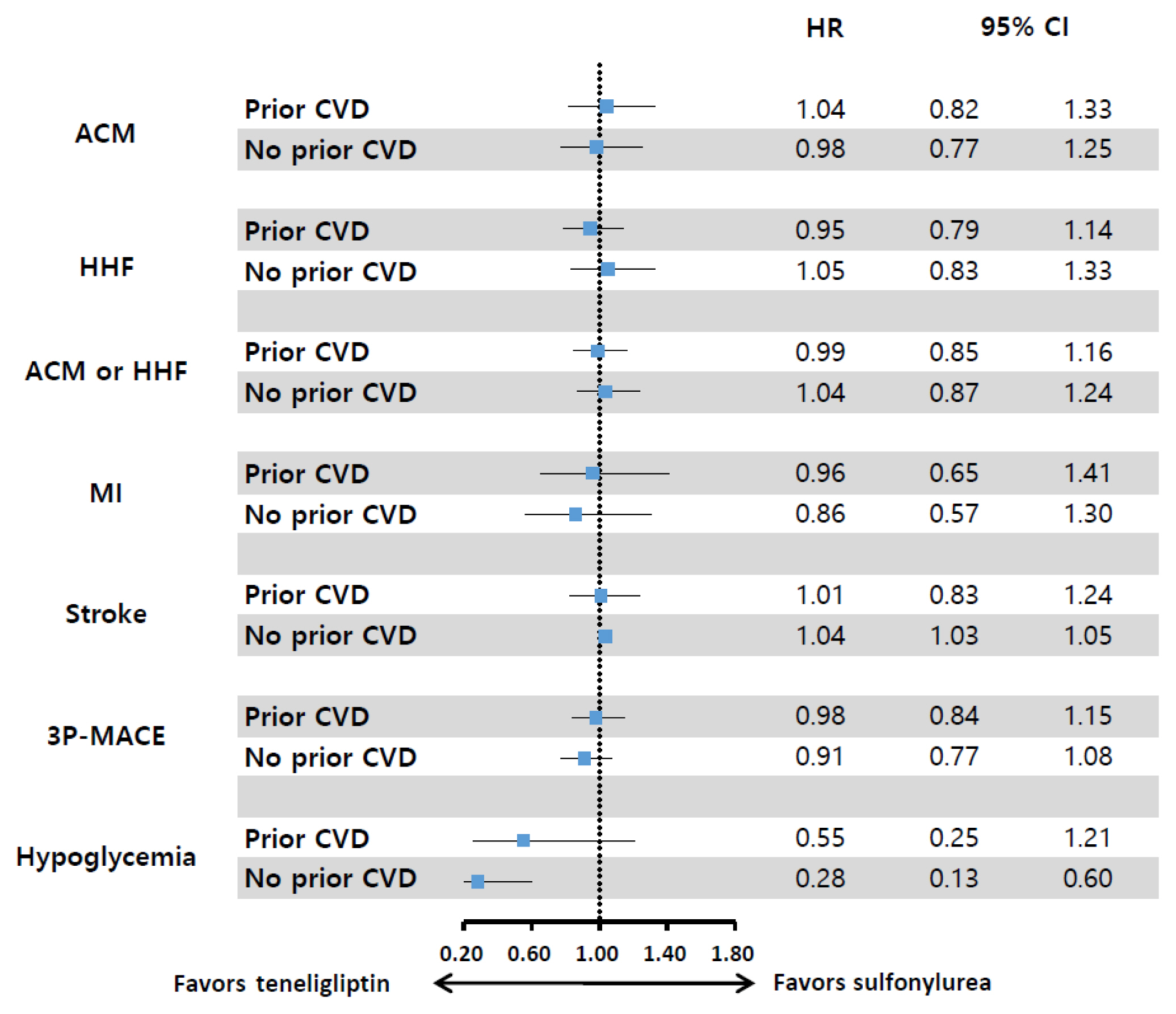
Results regarding the cardiovascular (CV) effects of dipeptidyl peptidase-4 (DPP-4) inhibitors are inconsistent. This study aimed to assess the effects of teneligliptin, a DPP-4 inhibitor, on the risk of major CV outcomes in type 2 diabetes mellitus (T2DM) patients compared to sulfonylurea.
Methods
From January 1, 2015 to December 31, 2017, we conducted a retrospective cohort study using the Korean National Health Insurance Service database. A total of 6,682 T2DM patients who were newly prescribed DPP-4 inhibitors or sulfonylurea were selected and matched in a 1:1 ratio by propensity score. The hazard ratios (HRs) for all-cause mortality, hospitalization for heart failure (HHF), all-cause mortality or HHF, myocardial infarction (MI), stroke, and hypoglycemia were assessed.
Results
During 641 days of follow-up, the use of teneligliptin was not associated with an increased risk of all-cause mortality (HR, 1.00; 95% confidence interval [CI], 0.85 to 1.19), HHF (HR, 0.99; 95% CI, 0.86 to 1.14), all-cause mortality or HHF (HR, 1.02; 95% CI, 0.90 to 1.14), MI (HR, 0.90; 95% CI, 0.68 to 1.20), and stroke (HR, 1.00; 95% CI, 0.86 to 1.17) compared to the use of sulfonylurea. However, it was associated with a significantly lower risk of hypoglycemia (HR, 0.68; 95% CI, 0.49 to 0.94) compared to sulfonylurea therapy.
Conclusion
Among T2DM patients, teneligliptin therapy was not associated with an increased risk of CV events including HHF, but was associated with a lower risk of hypoglycemia compared to sulfonylurea therapy. -
Citations
Citations to this article as recorded by- Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study
Da Hea Seo, Mina Kim, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes Research and Clinical Practice.2024; 208: 111098. CrossRef - Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes
R. Pelluri, S. Kongara, V. R. Nagasubramanian, S. Mahadevan, J. Chimakurthy
Journal of Endocrinological Investigation.2023; 46(5): 855. CrossRef - Finding the most cost-effective option from commonly used Dipeptidyl peptidase-4 inhibitors in India: a systematic study
Harmanjit Singh, Ekta Arora, Seerat Narula, Mandeep Singla, Armaan Otaal, Jatin Sharma
Expert Review of Endocrinology & Metabolism.2023; 18(4): 347. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef
- Association between age at diagnosis of type 2 diabetes and cardiovascular morbidity and mortality risks: A nationwide population-based study

- Clinical Study
- Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea
- Da Hea Seo, Shinae Kang, Yong-ho Lee, Jung Yoon Ha, Jong Suk Park, Byoung-Wan Lee, Eun Seok Kang, Chul Woo Ahn, Bong-Soo Cha
- Endocrinol Metab. 2019;34(3):282-290. Published online September 26, 2019
- DOI: https://doi.org/10.3803/EnM.2019.34.3.282
- 5,995 View
- 87 Download
- 15 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background This study investigated the overall status of diabetes control and screening for diabetic microvascular complications in patients with type 2 diabetes mellitus attending primary care clinics in Korea.
Methods In this cross-sectional observational study, 191 primary care clinics were randomly selected across Korea from 2015 to 2016. In total, 3,227 subjects were enrolled in the study.
Results The patients followed at the primary care clinics were relatively young, with a mean age of 61.4±11.7 years, and had a relatively short duration of diabetes (mean duration, 7.6±6.5 years). Approximately 14% of subjects had diabetic microvascular complications. However, the patients treated at the primary care clinics had suboptimal control of hemoglobin A1c levels, blood pressure, and serum lipid levels, along with a metabolic target achievement rate of 5.9% according to the Korean Diabetes Association guidelines. The screening rates for diabetic nephropathy, retinopathy, and neuropathy within the past 12 months were 28.4%, 23.3%, and 13.3%, respectively.
Conclusion The overall status of diabetes management, including the frequency of screening for microvascular complications, was suboptimal in the primary care clinics. More efforts should be made and more resources need to be allocated for primary care physicians to promote adequate healthcare delivery, which would result in stricter diabetes control and improved management of diabetic complications.
-
Citations
Citations to this article as recorded by- Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(6): 837. CrossRef - Effectiveness of quality of care for patients with type 2 diabetes in China: findings from the Shanghai Integration Model (SIM)
Chun Cai, Yuexing Liu, Yanyun Li, Yan Shi, Haidong Zou, Yuqian Bao, Yun Shen, Xin Cui, Chen Fu, Weiping Jia
Frontiers of Medicine.2022; 16(1): 126. CrossRef - Comparison of Health Outcomes by Care Provider Type for Newly Diagnosed Mild Type 2 Diabetes Patients in South Korea: A Retrospective Cohort Study
Hee-Chung Kang, Jae-Seok Hong
Healthcare.2022; 10(2): 334. CrossRef - Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Type 2 Diabetes Mellitus with Early Dry Skin Disorder: A Comparison Study Between Primary and Tertiary Care in Indonesia
Lili Legiawati, Kusmarinah Bramono, Wresti Indriatmi, Em Yunir, Aditya Indra Pratama
Current Diabetes Reviews.2022;[Epub] CrossRef - Long-Term Changes in HbA1c According to Blood Glucose Control Status During the First 3 Months After Visiting a Tertiary University Hospital
Hyunah Kim, Da Young Jung, Seung-Hwan Lee, Jae-Hyoung Cho, Hyeon Woo Yim, Hun-Sung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Effects of Diabetes Quality Assessment on Diabetes Management Behaviors Based on a Nationwide Survey
Chang Kyun Choi, Jungho Yang, Ji-An Jeong, Min-Ho Shin
International Journal of Environmental Research and Public Health.2022; 19(23): 15781. CrossRef - The Impact of the Indonesian Chronic Disease Management Program (PROLANIS) on Metabolic Control and Renal Function of Type 2 Diabetes Mellitus Patients in Primary Care Setting
Firas Farisi Alkaff, Fauzan Illavi, Sovia Salamah, Wiwit Setiyawati, Ristra Ramadhani, Elly Purwantini, Dicky L. Tahapary
Journal of Primary Care & Community Health.2021; 12: 215013272098440. CrossRef - Questionnaire-based Survey of Demographic and Clinical Characteristics, Health Behaviors, and Mental Health of Young Korean Adults with Early-Onset Diabetes
Ji In Park, Hyunjeong Baek, Sang-Wook Kim, Ji Yun Jeong, Kee-Ho Song, Ji Hee Yu, Il Sung Nam-Goong, Eun-Hee Cho
Journal of Korean Medical Science.2021;[Epub] CrossRef - Sodium–Glucose Cotransporter 2 Inhibitors and Risk of Retinal Vein Occlusion Among Patients With Type 2 Diabetes: A Propensity Score–Matched Cohort Study
Min-Kyung Lee, Bongsung Kim, Kyungdo Han, Jae-Hyuk Lee, Minhee Kim, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon, Young-Jung Roh
Diabetes Care.2021; 44(10): 2419. CrossRef - Challenges in the Management of Diabetes in Primary Care
Yeon Kyung Lee
The Journal of Korean Diabetes.2020; 21(3): 161. CrossRef - Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
Sung-Youn Chun, Dong Wook Kim, Sang Ah Lee, Su Jung Lee, Jung Hyun Chang, Yoon Jung Choi, Seong Woo Kim, Sun Ok Song
Diabetes & Metabolism Journal.2020; 44(6): 897. CrossRef - Comprehensive Efforts Are Needed to Improve the Quality of Primary Diabetes Care in Korea
Chan-Hee Jung
Endocrinology and Metabolism.2019; 34(3): 265. CrossRef
- Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study

- Clinical Study
- Effects of Single Vitamin D3 Injection (200,000 Units) on Serum Fibroblast Growth Factor 23 and Sclerostin Levels in Subjects with Vitamin D Deficiency
- Dongdong Zhang, Da Hea Seo, Han Seok Choi, Hye-Sun Park, Yoon-Sok Chung, Sung-Kil Lim
- Endocrinol Metab. 2017;32(4):451-459. Published online December 14, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.4.451
- 4,556 View
- 50 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Vitamin D deficiency remains common in all age groups and affects skeletal and non-skeletal health. Fibroblast growth factor 23 is a bone-derived hormone that regulates phosphate and 1,25-dihydroxyvitamin D homeostasis as a counter regulatory factor. 1,25-Dihydroxyvitamin D stimulates fibroblast growth factor 23 synthesis in bone, while fibroblast growth factor 23 suppresses 1,25-dihydroxyvitamin D production in the kidney. The aim of this study was to evaluate the effects of vitamin D3 intramuscular injection therapy on serum fibroblast growth factor 23 concentrations, and several other parameters associated with bone metabolism such as sclerostin, dickkopf-1, and parathyroid hormone.
Methods A total of 34 subjects with vitamin D deficiency (defined by serum 25-hydroxyvitamin D levels below 20 ng/mL) were randomly assigned to either the vitamin D injection group (200,000 units) or placebo treatment group. Serum calcium, phosphate, urine calcium/creatinine, serum 25-hydroxyvitamin D, fibroblast growth factor 23, sclerostin, parathyroid hormone, and dickkopf-1 levels were serially measured after treatment.
Results Comparing the vitamin D injection group with the placebo group, no significant changes were observed in serum fibroblast growth factor 23, parathyroid hormone, or dickkopf-1 levels. Serum sclerostin concentrations transiently increased at week 4 in the vitamin D group. However, these elevated levels declined later and there were no statistically significant differences as compared with baseline levels.
Conclusion Serum fibroblast factor 23, sclerostin, parathyroid hormone, and dickkopf-1 levels were not affected significantly by single intramuscular injection of vitamin D3.
-
Citations
Citations to this article as recorded by- Effect of vitamin D supplementation on circulating fibroblast growth factor-23 concentration in adults with prediabetes
Lisa Ceglia, Anastassios G. Pittas, Bess Dawson-Hughes
Aging Clinical and Experimental Research.2023; 35(3): 525. CrossRef - Fibroblast Growth Factor 23 in COVID-19: An Observational Study
Athena Myrou, Theodoros Aslanidis, Keli Makedou, Athanasios Mitsianis, Aikaterini Thisiadou, Paraskevi Karalazou, Georgios Chatzopoulos, Anastasios Papadopoulos, Antonios Kalis, Dimitrios Giagkoulis, Fotios Lezgidis, Christos Savopoulos
Cureus.2023;[Epub] CrossRef - The effect of vitamin D supplementation on serum levels of fibroblast growth factor- 23: A systematic review and meta-analysis of randomized controlled trials
Fatemeh Meshkini, Sepideh Soltani, Cain C.T. Clark, Vivian Tam, David Meyre, Omid Toupchian, Sahar Saraf-Bank, Shima Abdollahi
The Journal of Steroid Biochemistry and Molecular Biology.2022; 215: 106012. CrossRef - Serum sclerostin levels in osteoporotic fracture patients
Erwin A. Gorter, Casper R. Reinders, Pieta Krijnen, Natasha M. Appelman-Dijkstra, Inger B. Schipper
European Journal of Trauma and Emergency Surgery.2022; 48(6): 4857. CrossRef - Clinical Utility of Preoperative Vitamin D3 Injection for Preventing Transient Hypocalcemia after Total Thyroidectomy
Kwangsoon Kim, Cho Rok Lee, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Kee-Hyun Nam, Woong Youn Chung, Claudio Casella
International Journal of Endocrinology.2021; 2021: 1. CrossRef - The effect of vitamin D supplementation on fibroblast growth factor‐23 in patients with chronic kidney disease: A systematic review and meta‐analysis
Elmira Karimi, Sama Bitarafan, Seyed Mohammad Mousavi, Nikan Zargarzadeh, Pari Mokhtari, Jessie Hawkins, Alipasha Meysamie, Fariba Koohdani
Phytotherapy Research.2021; 35(10): 5339. CrossRef - Pharmacodynamics of Oral Cholecalciferol in Healthy Individuals with Vitamin D Deficiency: A Randomized Open-Label Study
Angelo Fassio, Davide Gatti, Maurizio Rossini, Camilla Benini, Elena Fracassi, Eugenia Bertoldo, Ombretta Viapiana, Stefano Milleri, Matteo Gatti, Giovanni Adami
Nutrients.2021; 13(7): 2293. CrossRef - Vitamin D Deficiency at Mid-Pregnancy Is Associated with a Higher Risk of Postpartum Glucose Intolerance in Women with Gestational Diabetes Mellitus
Kyung-Soo Kim, Seok Won Park, Yong-Wook Cho, Soo-Kyung Kim
Endocrinology and Metabolism.2020; 35(1): 97. CrossRef - Effects of vitamin D supplementation on bone turnover markers and other bone-related substances in subjects with vitamin D deficiency
Rolf Jorde, Astrid Kamilla Stunes, Julia Kubiak, Ragnar Joakimsen, Guri Grimnes, Per Medbøe Thorsby, Unni Syversen
Bone.2019; 124: 7. CrossRef - Vitamin D Enhances the Efficacy of Topical Artificial Tears in Patients With Dry Eye Disease
Jin Sun Hwang, Yoon Pyo Lee, Young Joo Shin
Cornea.2019; 38(3): 304. CrossRef
- Effect of vitamin D supplementation on circulating fibroblast growth factor-23 concentration in adults with prediabetes

- Site-Specific Difference of Bone Geometry Indices in Hypoparathyroid Patients
- Hye-Sun Park, Da Hea Seo, Yumie Rhee, Sung-Kil Lim
- Endocrinol Metab. 2017;32(1):68-76. Published online February 6, 2017
- DOI: https://doi.org/10.3803/EnM.2017.32.1.68
- 3,306 View
- 32 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Hypoparathyroid patients often have a higher bone mineral density (BMD) than the general population. However, an increase in BMD does not necessarily correlate with a solid bone microstructure. This study aimed to evaluate the bone microstructure of hypoparathyroid patients by using hip structure analysis (HSA).
Methods Ninety-five hypoparathyroid patients >20 years old were enrolled and 31 of them had eligible data for analyzing bone geometry parameters using HSA. And among the control data, we extracted sex-, age-, and body mass index-matched three control subjects to each patient. The BMD data were reviewed retrospectively and the bone geometry parameters of the patients were analyzed by HSA.
Results The mean Z-scores of hypoparathyroid patients at the lumbar spine, femoral neck, and total hip were above zero (0.63±1.17, 0.48±1.13, and 0.62±1.10, respectively). The differences in bone geometric parameters were site specific. At the femoral neck and intertrochanter, the cross-sectional area (CSA) and cortical thickness (C.th) were higher, whereas the buckling ratio (BR) was lower than in controls. However, those trends were opposite at the femoral shaft; that is, the CSA and C.th were low and the BR was high.
Conclusion Our study shows the site-specific effects of hypoparathyroidism on the bone. Differences in bone components, marrow composition, or modeling based bone formation may explain these findings. However, further studies are warranted to investigate the mechanism, and its relation to fracture risk.
-
Citations
Citations to this article as recorded by- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism
S. Saha, V. Mannar, D. Kandasamy, V. Sreenivas, R. Goswami
Journal of Endocrinological Investigation.2022; 45(9): 1777. CrossRef - Epidemiology and Financial Burden of Adult Chronic Hypoparathyroidism
Sigridur Bjornsdottir, Steven Ing, Deborah M Mitchell, Tanja Sikjaer, Line Underbjerg, Zaki Hassan-Smith, Jad Sfeir, Neil J Gittoes, Bart L Clarke L
Journal of Bone and Mineral Research.2020; 37(12): 2602. CrossRef - Effect of Endogenous Parathyroid Hormone on Bone Geometry and Skeletal Microarchitecture
A Ram Hong, Ji Hyun Lee, Jung Hee Kim, Sang Wan Kim, Chan Soo Shin
Calcified Tissue International.2019; 104(4): 382. CrossRef - Bone responses to chronic treatment of adult hypoparathyroid patients with PTH peptides
Sofie Malmstroem, Lars Rejnmark, Dolores M. Shoback
Current Opinion in Endocrine and Metabolic Research.2018; 3: 51. CrossRef
- Vertebral fractures, trabecular bone score and their determinants in chronic hypoparathyroidism


 KES
KES

 First
First Prev
Prev



